Navigating the tricky waters of managing a skin fungal infection, whether it presents as a persistent, itchy rash or a mysteriously flaky patch, can indeed be a source of stress and discomfort. These experiences, commonly encountered by a vast global population, not only warrant thorough attention but also a gentle approach to care. The silver lining here, amidst the anxiety these conditions may provoke, is that skin fungal infections are not only highly treatable but also preventable.
Fungi, specifically dermatophytes, announce their unwelcome presence when they penetrate the outer layer of the skin, hair, and nails, causing what is scientifically referred to as superficial mycoses. To comprehend the depth of these infections, it’s vital to realize that various types of fungi are behind these conditions, each presenting its unique set of symptoms, preferred infection sites, and expressions.
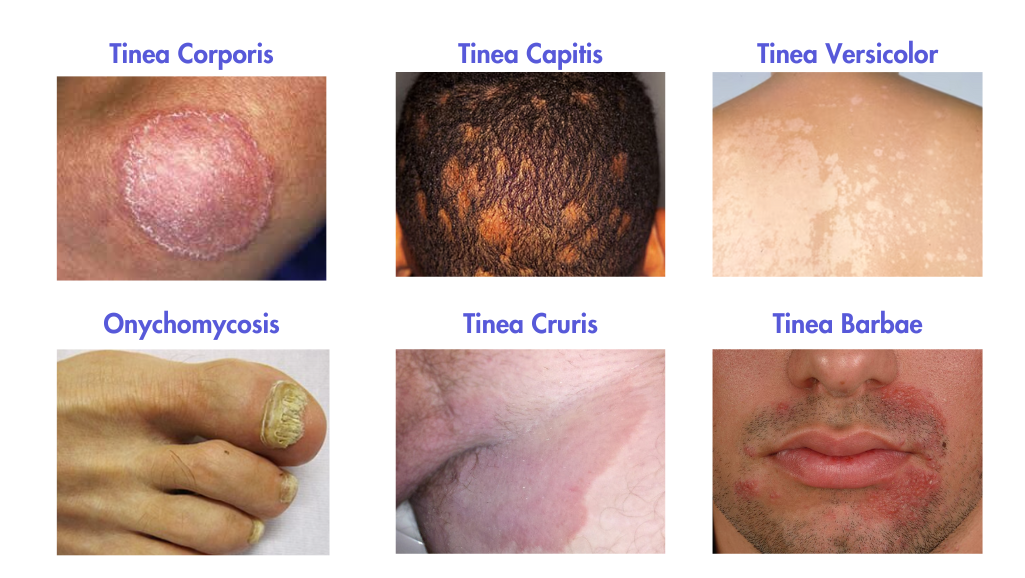
Exploring further into fungal infections, examples include tinea capitis, impacting primarily the scalp, tinea corporis or ringworm, identified by its notorious circular rash on the body, and tinea cruris, or “jock itch,” notorious for the insistent itch and redness it introduces to the groin area. Furthermore, trichophyton rubrum, amongst numerous species of dermatophytes, often emerges as a common adversary, causing everything from foot to nail fungus, but reassuringly, such conditions are commonplace and effectively treated by dermatologists around the world.
Identifying and Diagnosing Fungal Invaders
While skin fungal infections are nondiscriminatory, certain factors, including a weakened immune system, excessive sweating, dry skin, and specific lifestyle choices, notably enhance susceptibility to them. The first meeting with a fungal infection usually starts with a flat, red rash, which might be accompanied by a relentless itch or a burn. The symptoms, however, can vary, depending on the type and location of the infection.
When it comes to diagnosis, healthcare providers use a variety of tools and procedures to determine the exact nature of the condition. In many cases clinicians can evaluate and manage fungal infections without necessitating a physical consultation by examining photos that you submit. If you do need to be examined in-person then a dermatologist will use a dermatoscope (a magnified lens) to closely inspect the affected region. This examination might reveal distinctive characteristics, such as ‘comma hairs’ found in tinea capitis, offering vital clues to identifying the fungal antagonist at play.
Beyond visual examination, laboratory tests play a pivotal role in the diagnostic journey. The KOH preparation test, for instance, involves applying a solution to a skin scraping, subsequently examined under a microscope. This allows the practitioner to visualize the fungal elements in detail, providing insight into the species and strain at play.
Similarly, a skin culture, wherein a sample is allowed to cultivate in a controlled laboratory environment, can assist in identifying the fungal species and informing appropriate therapeutic strategies. Each of these methodologies aims at isolating and accurately identifying the fungal organism responsible for the visible dermatological distress. In certain intricate and stubborn cases, a skin biopsy may become necessitated to delve deeper into the skin’s layers and unravel the precise nature and extent of the infection. Here, a small skin sample is surgically removed and subjected to histopathological examination, offering a detailed insight into the cellular level and facilitating a more nuanced understanding of the fungal invasion.
Navigating Through Treatment and Prevention
The journey through the treatment and management of fungal infections is armed with well-researched and proven pharmaceutical options. It’s essential, however, to acknowledge that certain types of tinea, such as tinea capitis and onychomycosis, may prove stubborn adversaries.
Lifestyle adaptations are also integral to both management and prevention, where attention to daily habits, such as thorough drying of feet and careful navigation of public showers, can mitigate the risk of encountering fungi and ensure that treatment is not undermined by reinfection. Adherence to treatment is equally vital; resisting the urge to scratch and maintaining consistency in medication usage is pivotal for ensuring the thorough elimination of the fungal presence.
Although the journey through a skin fungal infection may indeed be unsettling, with prompt recognition, appropriate intervention, and armed with the right knowledge, effectively managing these dermatological challenges is entirely possible. Always prioritize consulting a dermatology provider for an accurate diagnosis and treatment, safeguarding the vibrant health of your skin.








