What is Atopic Dermatitis?
Atopic dermatitis (AD), also known as eczema, is a chronic skin condition characterized by intense itching, redness, and inflammation. It affects about 7.3% of the U.S. population, significantly impacting quality of life, including daily functioning, career opportunities, family dynamics, social relationships, and mental health.
Symptoms
Common symptoms include dry, cracked skin, and persistent itchiness, along with rashes that can appear swollen an  d change color depending on skin tone. Additionally, patients may experience small, raised bumps, oozing, crusting, and thickened skin.
d change color depending on skin tone. Additionally, patients may experience small, raised bumps, oozing, crusting, and thickened skin.
Other symptoms may involve darkening around the eyes and raw, sensitive areas caused by scratching. Atopic dermatitis often begins before the age of five and can persist into adolescence and adulthood, with periods of flare-ups followed by times of remission that may last for several years.
Triggers
The exact cause of atopic dermatitis is not fully known, but a combination of genetic and environmental factors is believed to contribute to this condition.
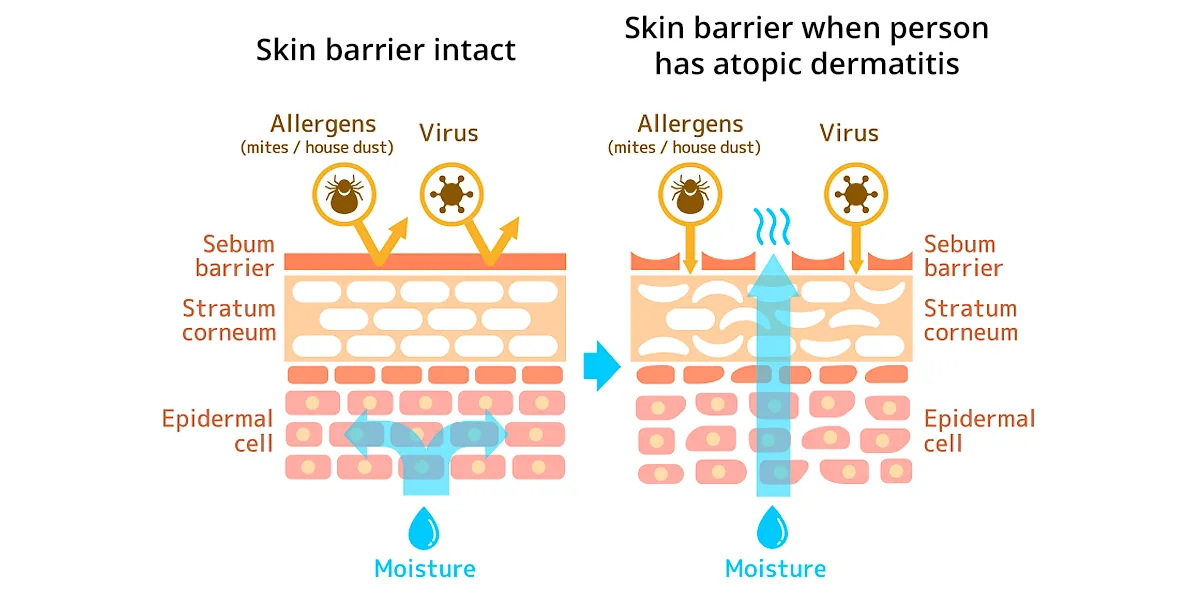
Genetic mutations, such as those in the filaggrin gene, weaken the skin barrier, which normally locks in moisture and blocks allergens and irritants. When this barrier is compromised, harmful substances can penetrate, leading to inflammation and dryness.
Environmental factors like house dust mites, pollen, pollution, and harsh soaps further damage the skin, while bacteria such as Staphylococcus aureus can worsen inflammation. Additionally, food allergies and stress can contribute to flare-ups, making proper skin care essential for maintaining a healthy barrier and preventing symptoms.
Diagnosis
The diagnosis of atopic dermatitis is generally clinical, meaning doctors identify it based on a physical examination of the skin and a discussion of your symptoms. Doctors may also ask about personal or family history of allergies, asthma, or eczema, as these conditions are often connected. While no specific test is required, additional tests like allergy testing or skin swabs may be done to rule out other conditions if needed. Recognizing the symptoms early can help with effective management and relief.
Management and Treatment
Atopic dermatitis is managed through a combination of medical treatment, skincare, and lifestyle changes.
Non-Medical Treatments:
Gentle skincare is crucial—using fragrance-free moisturizers, and mild cleansers helps maintain skin hydration. Identifying and reducing exposure to triggers, along with stress management, can help prevent flare-ups.
Topical and Systemic Treatments
Topical corticosteroids are often used first to reduce inflammation and itching, while topical calcineurin inhibitors (TCIs) are a non-steroidal option for sensitive areas. Antihistamines may help alleviate nighttime itching. For severe cases, systemic immunosuppressants like cyclosporine and methotrexate may be prescribed. More advanced treatments include dupilumab, an injectable biologic that reduces inflammation.
Effective atopic dermatitis management involves balancing medical treatments, daily skincare, and lifestyle adjustments to maintain skin health and reduce symptoms.
When should you see a medical professional?
You should see a medical professional if your atopic dermatitis symptoms are not improving with over-the-counter treatments, or if you have signs of infection, such as fever, redness, or pain. Regular check-ups are recommended if you have recurring flare-ups or if treatments need to be adjusted.