The link between Accutane and triglycerides is clear. Isotretinoin can increase blood fat levels during acne treatment. These changes often appear in the first few weeks and are usually mild. Still, they can sometimes lead to high cholesterol or pancreatitis if not monitored.
Dermatologists typically check baseline laboratory tests before starting treatment and repeat them frequently to monitor liver enzyme and triglyceride levels. Most people can safely stay on isotretinoin with medical supervision, a balanced diet, and healthy habits.
At DermOnDemand, board-certified dermatologists, such as Dr. Alicia Atkins, review each case to ensure every treatment is safe and personalized. Understanding how Accutane affects triglycerides helps patients stay informed, follow their plan, and protect their health during isotretinoin therapy.
Key Takeaways
- Accutane can temporarily raise triglyceride and cholesterol levels by affecting how the liver processes fats, making regular lab monitoring essential.
- Typical triglyceride levels should stay below 200 mg/dL during isotretinoin therapy, while levels above 500 mg/dL require immediate medical review to prevent pancreatitis.
- Baseline labs and follow-up testing every four to six weeks help detect early changes in triglycerides, liver enzymes, and cholesterol.
- Dietary changes, exercise, and, in some cases, omega-3 supplements or fibrates can help control high triglycerides without stopping treatment.
- Under dermatologist supervision, most patients complete isotretinoin therapy safely with personalized care and consistent monitoring.
Understanding the Role of Lipids in Acne Treatment
Isotretinoin works by shrinking oil glands and reducing sebum production, helping clear acne vulgaris. For a closer look at how this process affects oil balance, read more about Accutane and oily skin.
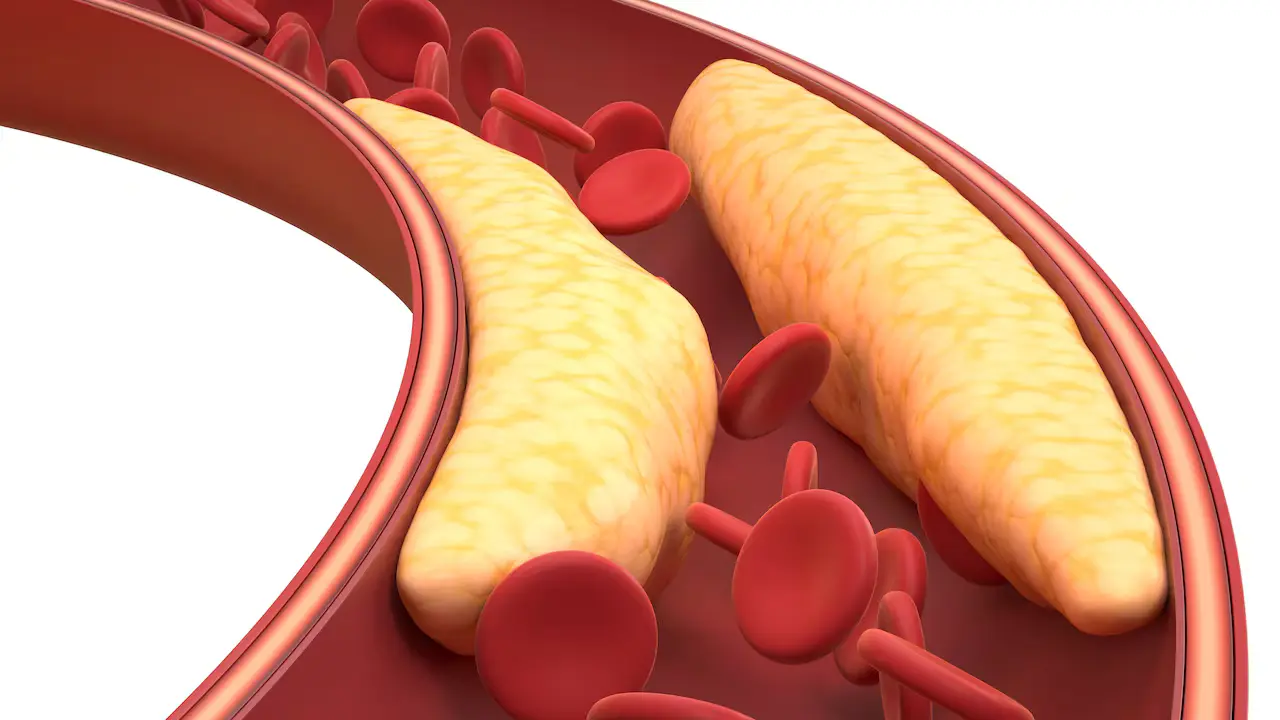
Sebum is composed of fats, so changes in how the body handles fats can impact both the skin and blood. Because Accutane alters how fats are processed, it can also affect cholesterol and triglyceride levels. This is why dermatologists closely monitor triglyceride levels and liver function during treatment.
How Accutane Affects Triglycerides and Cholesterol
Accutane can increase triglyceride and cholesterol levels in some individuals. It alters how the liver breaks down fats, leading to slight changes in blood lipids. Learn more about other common isotretinoin side effects that dermatologists monitor during treatment.
Does Accutane (Isotretinoin) Cause High Triglycerides?
Yes, it can. Isotretinoin therapy sometimes increases triglyceride levels, but most changes are mild and typically return to normal after treatment or with a lower dose. Because Accutane affects fat metabolism, it’s essential to conduct baseline labs before starting treatment and to monitor them regularly.
People with high cholesterol or metabolic issues may be at higher risk. Regular lab tests help doctors keep triglyceride levels within a safe range.
Why Triglyceride and Cholesterol Levels Increase
Accutane reduces oil in the skin but can also affect liver enzymes that handle fat. This can lead to higher levels of triglycerides and cholesterol. Most increases are small, but poor diet, alcohol use, or liver problems can make them worse.
Since Accutane is metabolized in the liver, regular liver enzyme tests are part of the care regimen. If the results change significantly, your dermatologist may adjust the dose or test more frequently.
Elevated Triglycerides During Accutane Treatment

Some patients experience higher triglyceride levels after a few weeks on Accutane. This doesn’t always mean stopping treatment, but it does require closer follow-up.
Typical Triglyceride Levels and Sudden Spikes
During isotretinoin therapy, mild increases in triglycerides are common and usually return to normal after treatment ends. Typical triglyceride levels range from less than 150 mg/dL (normal) to 150–199 mg/dL (borderline high).
Levels between 200–499 mg/dL are considered high, and anything above 500 mg/dL is very high and may raise the risk of pancreatitis.
If triglyceride levels rise sharply, your dermatologist will act quickly by reviewing recent lab results, diet, and medication use to find the cause and adjust your care plan.
Alcohol, processed foods, and missed lab checks can make levels climb faster. Keeping up with regular tests, limiting sugar and alcohol, and following a balanced diet help keep triglyceride levels in a safe range throughout treatment.
Other Medications That Raise Triglycerides
Certain medications, including corticosteroids, beta-blockers, and oral estrogens, can also increase triglyceride levels. When used in conjunction with Accutane, this effect can be more pronounced. Inform your dermatologist about all your medications so they can adjust your treatment plan safely and effectively.
How to Prepare for Isotretinoin Therapy
Before starting Accutane, dermatologists order baseline labs to check triglyceride, cholesterol, and liver enzyme levels. These tests establish a clear baseline for comparison as treatment progresses. Patients should also share all medications, alcohol use, and any family history of lipid problems.
To stay safe and get good results, patients should:
- Eat a low-sugar, low-alcohol diet.
- Drink enough water and eat regular meals.
- Get lab tests on schedule to catch early changes.
Proper preparation helps the skin and body adjust to isotretinoin therapy, thereby reducing the risk of side effects later.
Managing High Triglycerides on Accutane
When high triglycerides appear during Accutane treatment, dermatologists focus on controlling the rise early and keeping levels within a safe range. The goal is to strike a balance between achieving clear skin results and maintaining overall health and safety.
Doctors begin by reviewing lab results, lifestyle habits, and any medications that may worsen lipid levels. Based on this review, they may adjust the Accutane dose, recommend diet changes, or schedule more frequent blood tests.
With proper monitoring and small adjustments, most patients can continue isotretinoin therapy safely without interrupting their progress.
Can You Take Accutane with High Triglycerides?
Sometimes yes. If triglycerides are only slightly elevated, doctors may continue isotretinoin therapy with diet modifications and more frequent monitoring. If levels exceed the safe range, treatment may be paused until they return to normal.
Monitoring Frequency and Safe Ranges
Doctors typically review laboratory results before starting treatment and every 4 to 6 weeks afterward. This includes triglycerides, cholesterol, and liver enzymes.
Safe triglyceride levels are below 200 mg/dL during therapy. If results are higher, doctors may lower the dose or test every two weeks until levels improve.
Diet, Exercise, and Medical Adjustments
Healthy habits help control triglycerides. Patients should:
- Avoid alcohol, fried foods, and processed snacks.
- Eat more fish, nuts, and other omega-3–rich foods.
- Exercise regularly to support heart and liver health.
If lifestyle changes don’t help enough, short-term medication can safely lower triglycerides under a doctor’s care.
When to Stop or Adjust Accutane for Triglycerides
Knowing when triglycerides are too high helps prevent problems. Dermatologists use lab results and symptoms to determine whether treatment should be continued, changed, or paused.
Warning Signs and Dermatologist Recommendations
If your triglyceride levels exceed 500 mg/dL or you experience symptoms such as stomach pain, nausea, or fatigue, contact your doctor immediately.
Dr. Atkins and the DermOnDemand team recommend checking labs again in these cases. The doctor may lower the dose or temporarily stop treatment until your levels return to normal.
Isotretinoin Triglycerides Treatment Options
If triglyceride levels stay high even after improving diet and exercise, dermatologists may recommend additional support. Short-term use of fibrates or prescription-strength omega-3 supplements can safely and effectively lower blood fat levels.
These medications reduce the risk of pancreatitis and allow patients to continue isotretinoin therapy without interruption. Each case is carefully reviewed to strike a balance between skin improvement and long-term health, and treatment plans are adjusted as soon as lab results indicate improvement.
When to Resume Accutane After Levels Normalize
Once triglycerides return to a healthy range, most patients can restart Accutane under close medical supervision. Dermatologists often start with a lower dose and recheck triglyceride levels within two to four weeks.
If results remain stable, therapy continues with regular lab testing every few weeks. This step-by-step approach ensures the medication remains effective while maintaining safe lipid levels and liver function.
Reducing Risks for Safer Treatment
DermOnDemand designs every isotretinoin plan to match the patient’s unique health profile. Regular checkups, lab reviews, and small dosage adjustments help prevent side effects and maintain safety throughout treatment.
Under the care of Dr. Alicia Atkins and her team, patients receive expert guidance throughout their treatment. For patients curious about different acne medications, our detailed comparison of isotretinoin vs tretinoin explains how each treatment works and when dermatologists recommend them.
How Dermatologists Monitor and Prevent Complications
Dermatologists test cholesterol and triglyceride levels often to spot small changes early. They also monitor liver enzymes to ensure the body handles Accutane safely. Open communication between the patient and the doctor helps fix issues before they become serious.
Patients who follow their care plan and maintain a healthy lifestyle typically complete treatment without complications. Under the care of Dr. Alicia Atkins and her team, patients receive expert guidance throughout their treatment.
Key Tips for Safe Use
- Obtain baseline laboratory tests before initiating isotretinoin therapy.
- Go to every follow-up visit for lab checks.
- Inform your dermatologist about all medications and supplements you are currently taking.
- Eat well and exercise to maintain healthy triglyceride levels.
- Report any new symptoms or side effects right away.
FAQs About Accutane and Triglycerides
For most patients, changes in triglyceride levels are temporary. Levels usually return to normal a few weeks after stopping isotretinoin therapy. Long-term effects are rare when treatment is properly supervised and laboratory abnormalities are monitored closely.
A triglyceride level below 200 mg/dL is generally considered safe. Higher values warrant closer follow-up by your dermatologist.
Yes, but only in severe cases. If triglyceride levels exceed 500 mg/dL, dermatologists may pause or adjust therapy to prevent complications like pancreatitis. With proper monitoring, most patients can safely resume treatment after they have stabilized.
Most dermatologists test triglyceride levels before treatment begins and then repeat the test every four to six weeks thereafter. If results indicate a rise or if risk factors are present, testing may be conducted more frequently to ensure patient safety.
Yes. Once treatment ends, triglyceride and cholesterol levels typically return to normal within a few weeks. Healthy eating and exercise can help the body restore balance faster.
Start Your Dermatologist-Guided Accutane Plan
If you’re considering isotretinoin therapy or need expert guidance on managing triglyceride levels safely, connect with DermOnDemand today. Dr. Alicia Atkins and her team provide personalized, prescription-grade care without waiting rooms or delays.
Book your private online consultation and get a treatment plan reviewed by a board-certified dermatologist within 24 hours.
This article provides general information and should not be used as a substitute for medical advice.