What is keratosis pilaris?
Keratosis pilaris (KP) is a prevalent dermatological condition characterized by the buildup of keratin within hair follicles, leading to a distinctive bumpy texture of the skin’s surface. This gives rise to its common names such as “chicken skin” or “goosebump skin.” It affects 50-80% of adolescents and 40% of adults. The most affected areas include the thighs, buttocks, and upper arms. Beginning in childhood, KP becomes more noticeable during adolescence and adulthood, persisting throughout life. It often peaks during winter months due to factors such as dry air and reduced humidity levels. Despite its appearance, KP is benign in nature, causing no harm. However, individuals affected by KP may experience frequent medical appointments due to cosmetic concerns, which can also result in psychosocial impacts, such as lowered self-esteem or social discomfort. In rare cases, KP may be associated with other medical conditions or syndromes.
What are the causes of KP? 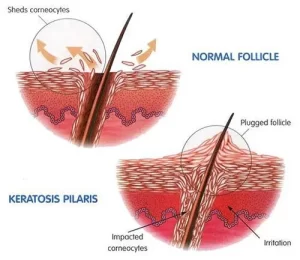
The exact causes of KP are poorly understood. It occurs due to abnormal trapping of keratin in the hair follicles. Nearly 40% of patients have a family history of KP.
What are the symptoms of KP?
KP presents with small rough keratoses (bumps) around the hair follicles that are dry and can vary in color, appearing skin-colored, red, or brown depending on the individual’s skin tone. In lighter skin tones, these bumps tend to be red, while in darker skin tones, they may appear brown or black. These bumps may also be dry, itchy, and accompanied by erythema (redness). Typically found on the extensor surfaces of the arms, lower legs and thighs, KP can affect other areas of the body as well. Despite being harmless, KP has the potential to lead to complications such as scarring, atrophy, and hair loss.
What are the clinical variants of KP?
There are several subtypes of KP, each displaying distinct characteristics. Keratosis pilaris rubra, for example, is marked by prominent redness around the hair follicles on the cheeks, forehead, and neck. Another variant, erythromelanosis follicularis faciei et colli, presents with redness, increased pigmentation, and small keratotic bumps on the face, neck, and extensor surfaces of the arms. This subtype of KP tends to be more prevalent among adolescents and young adults.
How is KP diagnosed?
KP is a clinical diagnosis, however physicians can utilize tools such as dermoscopy and biopsy to support the diagnosis if necessary. KP frequently coexists with other skin conditions, such as atopic dermatitis, ichthyosis vulgaris, folliculitis, and milia. Moreover, there have been reports linking KP with obesity, type 1 diabetes mellitus, pregnancy, as well as syndromes such as Down syndrome and Noonan syndrome.
KP is highly prevalent, yet it shares similarities with several other skin conditions, leading to potential misdiagnosis. For example, it can be confused with lichen spinulosus, phrynoderma, and keratosis pilaris atrophicans. Lichen spinulosus, typically observed in children, manifests symmetrically across the trunk and extremities with rough bumps that merge into larger lesions, distinguishing it from KP. Phrynoderma, another condition resembling KP, arises from vitamin A deficiency or general malnutrition. Keratosis pilaris atrophicans comprises a group of disorders characterized by atrophy, scarring, and hair loss.

What is the treatment for KP?
While there is currently no cure for KP, the condition is benign and typically does not necessitate treatment. Furthermore, KP often improves on its own as individuals age. However, for those who are troubled by its cosmetic appearance, there are various over-the-counter (OTC) and prescription treatments available. These options can help alleviate symptoms and improve the appearance of the skin affected by KP.
Topicals
The initial approach to treating KP typically involves the use of skin exfoliants such as lactic acid (ammonium lactate) and emollients containing urea and salicylic acid. Lactic acid helps to loosen up the scales and promote smoother skin texture while moisturizers with urea and salicylic acid provide hydration, soften the skin, and protect the skin barrier. Research has demonstrated that creams containing 20% urea applied to affected areas for a duration of 4 weeks can effectively enhance the appearance of the skin. It is essential to note that any improvements achieved through these treatments are usually temporary. Patients who respond well to treatment are encouraged to maintain long-term use to sustain results.
If initial treatments prove ineffective, patients may turn to topical retinoids such as tretinoin 0.05%, adapalene 0.1%, or tazarotene 0.05%. These medications are typically applied once daily and should be continued for 2-3 months.
Topical steroids can also be incorporated into treatment regimens alongside other agents to address inflammation, redness, and itching associated with KP. These medications are applied once or twice daily to affected areas and are typically used for a duration of up to 2 weeks.
Other Options
Additional treatment options for KP include systemic retinoids, laser therapies such as Q-switched Nd:YAG lasers and combination laser treatments, as well as microdermabrasion. Intense pulsed light and pulse dye laser have shown promising results in treating the erythema associated with KP, as evidenced by successful outcomes in clinical settings. These modalities can help reduce redness and improve the overall appearance of affected skin areas. CO2 lasers are particularly beneficial for treating atrophy and scars associated with KP.
Takeaways
Keratosis pilaris is a prevalent skin condition characterized by follicular keratinization, manifesting as rough, spiny keratotic papules primarily on the extensor surfaces of the arms and thighs. It can also affect areas such as the face, trunk, and buttocks. KP typically appears in childhood or adolescence and often improves with age. It is commonly associated with atopic dermatitis and ichthyosis vulgaris and may occur alongside other diseases or syndromes. Diagnosis of KP relies on clinical presentation and medical history. While KP itself is benign and tends to improve on its own over time, individuals with cosmetic concerns may find relief using emollients and topical keratolytics. For those who do not respond to initial treatments, topical retinoids are considered a second-line therapy. For more resistant forms of KP, or cases involving scarring and atrophy, lasers and combination therapies can be used effectively. These modalities aim to alleviate symptoms and enhance the appearance of affected skin areas.