Rosacea, eloquently pronounced “row-ZAY-sha,” is a widespread and chronic inflammatory skin condition, affecting a staggering 16 million people in the United States and over 415 million worldwide. Characterized by persistent facial redness, visible blood vessels, and occasionally, the appearance of small, pimple-like bumps, rosacea becomes a lifelong companion for those it touches. Predominantly surfacing in adulthood and frequently observed in fair-skinned women, it nevertheless extends its impact across all genders, races, and ages, demonstrating its nondiscriminatory nature. While its exact origins remain shrouded in mystery, thought to be a confluence of genetic, environmental, and vascular factors, its presence is undeniably apparent. Despite lacking a definitive cure, a deep understanding, precise diagnosis, and suitable treatments enable effective management of its symptoms, guiding those affected on their continual journey with this pervasive skin disorder.
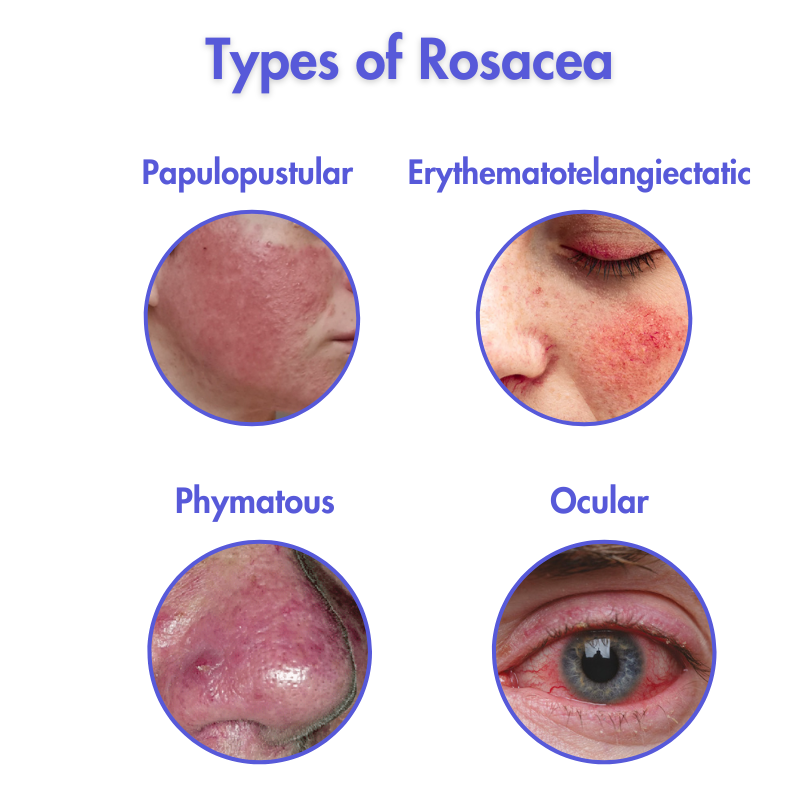
The complexity of rosacea is manifested through its various forms, encapsulating four primary types:
- Erythematotelangiectatic Rosacea: Notable for persistent facial redness and enlarged, visible blood vessels, with symptoms that can unexpectedly wax and wane.
- Papulopustular Rosacea: Characterized by the presence of pus or fluid-filled pimples that may resemble acne, coupled with skin swelling.
- Phymatous Rosacea: Inducing skin thickening and swelling, particularly impacting the nose, potentially culminating in a bulbous appearance, termed rhinophyma.
- Ocular Rosacea: Affecting the eyes, it brings about irritation, redness, and watery eyes, with painful bumps, known as styes, forming on the eyelids.
Clinical Presentation of Rosacea
Rosacea presents in several ways, with common primary features including persistent facial redness, flushing or blushing easily, and visible blood vessels (telangiectasia). Secondary features may include the development of papules (small red bumps), pustules (pus-filled bumps), and the enlargement of oil glands, leading to a condition called rhinophyma. These symptoms tend to wax and wane, occurring in flare-ups that can be triggered by certain foods, alcohol, temperature extremes, stress, and UV exposure.
The initial characterization of rosacea often involves discerning specific manifestations on the skin. Transient erythema, characterized by episodic facial redness or flushing, can often be triggered by a range of factors, such as diet, stress, or temperature changes. This becomes a notable feature, given its sporadic yet prominent appearance. In contrast, persistent erythema presents as a more continuous, seemingly unyielding redness, typically inhabiting central facial regions like the cheeks, nose, and forehead, thereby establishing itself as a resilient and visually apparent symptom.
Inflammatory papules and pustules, bearing semblance to acne lesions, introduce another layer of complexity. These red, pus-filled bumps act as both a visual and physical symptom, sometimes causing discomfort or sensitivity. Additionally, telangiectasia, or the manifestation of visible blood vessels or dilated capillaries on the skin’s surface, further complicates the patient’s experience and serves as another critical diagnostic criterion.
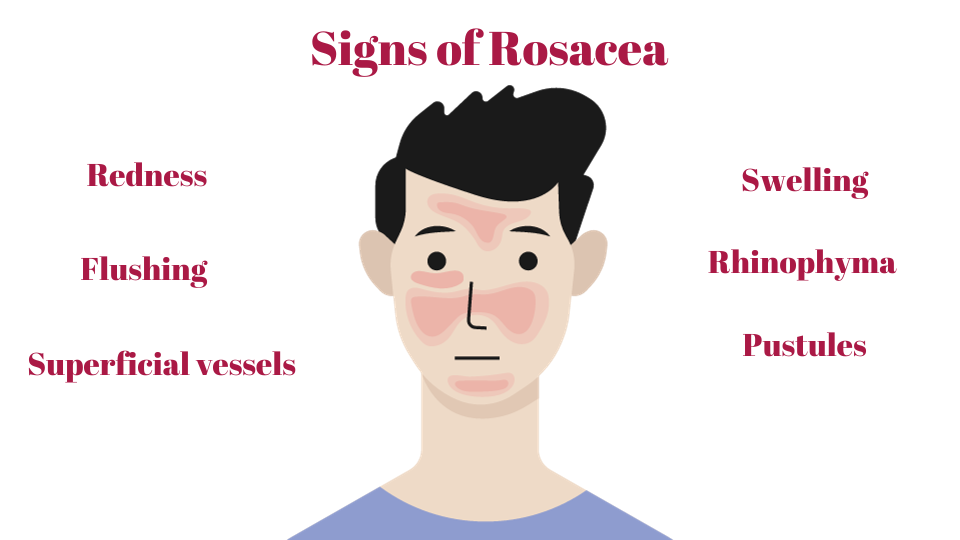
Diving deeper, rosacea may express itself through secondary features, which can independently or collectively surface. Phymatous changes, for instance, involve the thickening of the skin, often heralding a bumpy or enlarged appearance, most commonly manifesting on the nose (a condition known as rhinophyma). This physical alteration not only impacts aesthetic aspects but can also influence self-perception and interpersonal interactions.
Concurrently, individuals may navigate through sensations of burning or stinging, presenting an invisible yet palpable struggle. Similarly, erythematous plaques, or red skin patches, join the fray, often uninvited, adding to the mosaic of rosacea’s presentation. Facial dryness and scaling provide another tier, revealing dry, flaky skin that can be both visually and physically disruptive. Edema, particularly centralized facial swelling, might also emerge, introducing both aesthetic and comfort-related challenges.
Rosacea doesn’t confine itself strictly to facial symptoms. It may extend its reach to peripheral locations, affecting areas beyond the visage. Furthermore, ocular manifestations such as redness, dryness, and irritation of the eyes also weave themselves into the tapestry of rosacea’s clinical picture, necessitating comprehensive care that spans dermatological and potentially ophthalmological management.
Distinguishing Rosacea from Acne Vulgaris
While rosacea shares symptomatic similarities with Acne Vulgaris (common acne), they are notably disparate conditions. Acne usually surfaces during adolescence, instigated by hormonal changes, and features distinct elements such as comedones (blackheads and whiteheads), papules, pustules, and nodules on the face, chest, back, and shoulders. In contrast, rosacea often emerges post-30, is localized predominantly on the face, and is typically devoid of comedones. Its triggers differ, often involving elements like sunlight exposure, spicy foods, and stress, thus providing clear distinctions in their causes, onset ages, and predominant clinical features.
Causes of Rosacea
The exact cause of rosacea remains elusive, but it is believed to involve a combination of factors. Possible contributors include genetic factors, immune system dysfunction, vascular changes, and inflammation. Certain factors such as the presence of microscopic skin mites known as Demodex, UV exposure, diet, and stress may also trigger rosacea or worsen current symptoms.
- Genetic Predisposition: genetics may play a significant role in the development of rosacea. Recent studies strongly support familial inheritance of and show that genetics may contribute up 46% to the development of rosacea
- Immune System Dysregulation: At the heart of rosacea lies an intricate interplay within your immune system. With rosacea, certain immune cells, such as keratinocytes, endothelial cells, macrophages, and dendritic cells, along with adaptive immune cells like T helper (Th)1 cells, Th17 cells, and plasma cells, exhibit a state of miscommunication. This immune “overactivity” results in inflammation within your skin, akin to an overzealous defense mechanism that inadvertently targets your skin. Rosacea patients typically display elevated levels of metalloproteinases (MMPs) and overexpression of Toll-like receptor 2 (TLR2). These Inflammatory factors, including the release of cytokines, play a role in the formation of papules and pustules
- Vascular Abnormalities: Rosacea’s signature redness and visible blood vessels are attributed to vascular abnormalities. Your skin normally has a system for regulating blood flow, ensuring it doesn’t overreact to various stimuli. In rosacea, this regulatory system malfunctions. Blood vessels in your skin dilate excessively, causing persistent erythema (redness) and telangiectasia (the appearance of visible blood vessels).
- Neurovascular Interaction: Rosacea is also influenced by your nervous system. The skin is densely populated with nerve endings, and with rosacea, these nerve endings become more active. They release neuropeptides, which are small molecules that act as signaling agents. These overactive neuropeptides play a role in the heightened sensitivity and the chronic and exaggerated local inflammatory response in the skin. This includes flushing (sudden redness), burning sensations, and heightened skin sensitivity.
- Environmental Trigger Factors of Rosacea: While the precise cause of rosacea remains elusive, certain factors can trigger or worsen its symptoms. Ultraviolet (UV) radiation from the sun is a well-documented trigger, causing inflammation, neoangiogenesis (formation of new blood vessels), telangiectasia (dilation of blood vessels), and fibrosis. Air pollution and smoking can also contribute to skin damage and exacerbate rosacea. Nutrition, stress, and heat are additional factors that may trigger or worsen rosacea symptoms. Specific nutrition triggers may include: alcohol, hot beverages, spicy food (capsaicin), fatty food, and those containing cinnamaldehyde such as chocolate, tomatoes, and citrus. However, increased coffee consumption may decrease risk of rosacea development.
Recent research also suggests an association between rosacea and depression, anxiety disorder, hypertension (high blood pressure), cardiovascular diseases, dyslipidemia (high cholesterol), diabetes mellites, migraine, rheumatoid arthritis, Helicobacter pylori infection, ulcerative colitis, and dementia. However, no causative links have been drawn, and the risk of developing co-morbid diseases varies for each individual. Patients are strongly advised to consult their dermatologist regarding their risk for developing co-morbid diseases.
Treating Rosacea
Managing rosacea demands a comprehensive and multifaceted strategy that includes crucial lifestyle modifications. Avoiding recognized triggers like spicy foods, alcohol, and severe temperatures is crucial. Similarly, mindful dietary choices, such as avoiding hot beverages, play a pivotal role in mitigating the likelihood of flare-ups. It is imperative to underscore the significance of patient education in this context. Ensuring that patients have a thorough understanding and adherence to these essential management strategies becomes an integral part of comprehensive rosacea care.
Treatment choices for rosacea hinge heavily on the specific subtype and severity of the condition, necessitating a broad spectrum of therapeutic interventions. Non-pharmacologic skin care often centers around gentle cleansing practices that circumvent mechanical damage, chemical irritation, and pH disruption, given the compromised skin barrier inherent in rosacea. The choice of moisturizers—non-oily and fragrance-free—targets alleviation of dryness and barrier restoration, while a simplified skincare regimen minimizes the potential for irritant or allergic responses. Additionally, daily application of broad-spectrum sunscreen with at least SPF 30 and the incorporation of anti-inflammatory and skin-calming ingredients becomes a staple in routine skin care.
Topical and Oral Therapies: Moving to the realm of pharmacological interventions, topical therapies, including antibiotics and retinoids, are commonly enlisted to manage inflammation and control skin texture. On the other hand, oral medications—ranging from antibiotics for moderate to severe conditions, anti-inflammatories in specific circumstances, to isotretinoin for severe, non-responsive cases—broaden the therapeutic approach. Notably, the role of isotretinoin underscores the need for meticulous monitoring due to its potential side effects.
Leveraging Light and Laser Therapy: Light and laser therapy, incorporating interventions like Intense Pulsed Light (IPL) and targeted laser therapy, offer a valuable toolset for managing persistent redness and visible blood vessels. These strategies not only alleviate current symptoms but also provide a proactive approach to managing the potential aesthetic impact of the condition over time.
Lifestyle Modifications: Lifestyle modifications, from ensuring robust sun protection through clothing and SPF to adopting a gentle skincare routine, emerge as cornerstone strategies. Stress management also weaves into this tapestry, wherein techniques like yoga and meditation might offer additional relief by mitigating stress-induced exacerbations. Furthermore, understanding that rosacea manifests uniquely across individuals propels healthcare providers toward adopting personalized approaches to both diagnosis and treatment. Working in tandem with a dermatologist to sculpt a treatment plan that is exquisitely tailored to specific symptoms and triggers becomes pivotal.
Emergent research is progressively illuminating the underpinnings of rosacea, paving the way for potentially transformative treatments in the future. Insights into the roles of Demodex mites and the skin microbiome are unearthing new management paradigms. Moreover, promising therapies, including those that harness specific pathophysiological mechanisms, offer a beacon of hope for more personalized and effective treatment regimens. The exploration into novel therapies, such as the application of botulinum toxin (Botox), albeit in its early stages, opens up a promising trajectory towards more diverse and efficacious treatment options in rosacea management.








