What is stasis dermatitis?
Stasis dermatitis, also called gravitational dermatitis, venous eczema or venous stasis dermatitis, is a condition that involves skin changes that are the result of high venous pressures caused by venous reflux. This can be due to a weakening of the valves of the leg veins that help push blood back to the heart, allowing fluid to leak into the surrounding interstitial space. Eventually fluid will end up pooling in the legs and causing skin changes. This condition most often develops as a person ages, but it could also be a sign of kidney or heart disease.
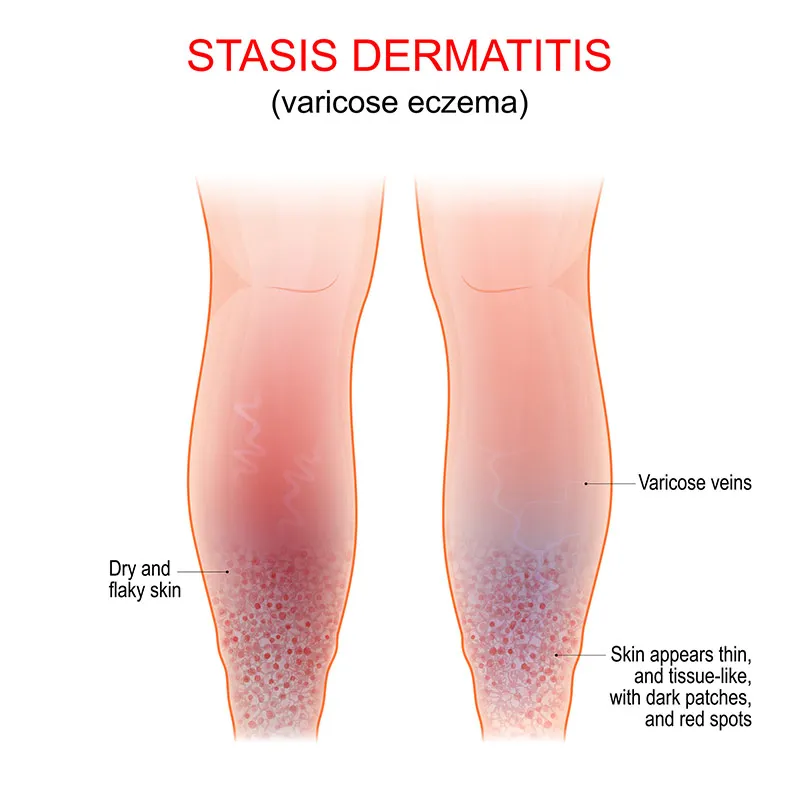
What are common symptoms of stasis dermatitis? 
Stasis dermatitis mainly affects the ankles due to how they are affected by gravity. Symptoms are as follows:
- Dry, itchy, discolored skin
- Skin aches and feels heavy, especially when standing or walking
- Swelling that is most prominent at the end of the day or when standing/walking
- Skin can thicken, get darker, look scaly, get dark speckles, and even elicit pain
- Wounds or sores can develop on the area
- The wounds can eventually get infected if not treated
- The area can get larger or spread to other regions
- You may see a person with stasis dermatitis have spider veins or varicose veins in neighboring regions of the body
Who gets stasis dermatitis?
Stasis dermatitis can happen after chronic valve reflux or insufficiency. Due to the nature of this condition, it is most often observed in older populations as this condition develops over a long period of time. It is also seen more often in females, because their valves are smaller than their male counterparts, and a certain amount of damage is more likely to have an impact on a smaller valve than a larger valve. Being overweight also puts someone at a greater risk. People who stand and or sit for long periods of time without movement or compression are at a greater risk. Stasis dermatitis has also been noted to have a higher prevalence in Western countries.
Some medical conditions will also put someone at a greater risk including
- Past leg surgery
- Hypertension
- Congestive heart failure
- Family history of valvular conditions
- Past history of blood clots
- Varicose veins
- Past history of leg ulcers
- History of edema in legs
- Pregnancy
- Kidney disease
What are treatment options for stasis dermatitis?
The best treatment for stasis dermatitis would be to treat the underlying cause. This may include going to a vascular specialist, and if ulcers are present, going to a wound care specialist. Do not neglect going to a primary care physician, and any other specialists for other chronic conditions as well. This includes taking prescribed medications, getting lab work and necessary scans. A doctor may ask to get an ultrasound to visualize valve flow. Physicians need to distinguish between stasis dermatitis and other conditions, such as cellulitis. Therefore, it is important to give an accurate past medical history including conditions, medications, past surgeries and injuries.
Your dermatologist may recommend:
- Compression stockings of at at least 8-15 mmhg pressure (a higher recommendation may yield better results, but a lower compliance rate. It is best to start from 8-15 mmhg and try different pressures to see which one will yield best compliance)
- Elevating your legs above your heart when you sleep and throughout the day
- Exercising, staying at a healthy weight, taking breaks from standing
- Low salt diet to help control the swelling
- Moisturizer and an occlusive petrolatum jelly on top for dryness
- Steroids or antihistamines if the area is itchy
- Topical calcineurin inhibitors (note they can cause burning sensation upon application)
- If there is a wound, daily would cleaning and topical antibiotics to prevent infection
- Pentoxifylline is a platelet aggregation inhibitor that can aid in ulcer healing due to improving microcirculation and decreasing viscosity
- Hydroxyethylrutosides can may be used to improve pain, cramps, and feeling of heaviness in legs
- Discussing switching medications that can cause the edema (i.e. calcium channel blockers)
- For varicose and spider veins, one might consider a procedure called sclerotherapy where a needle is used to inject a solution into the vein which will help it appear smaller
- Surgery may be needed to address the underlying cause
Takeaway message
It is important to recognize the early signs of stasis dermatitis before they become chronic. Once discovered, venous stasis is a sign of valvular insufficiency which although it can be a benign lifelong condition, people with this insufficiency are at a greater risk of deep vein thrombosis. Make sure to tell your healthcare providers your complete history in order to get the best care you need. There are a variety of treatment options for stasis dermatitis based on a person’s presentation, how invasive the treatment they are interested in, and if they are a candidate for said treatment. Consider seeing a dermatologist to improve both the cosmetic and functional symptoms of this condition.