The link between Accutane and PCOS is well-known among dermatologists. Isotretinoin, also called Accutane, helps women who struggle with acne caused by hormonal imbalance due to polycystic ovary syndrome (PCOS).
It reduces oil, inflammation, and clogged pores, allowing the skin to remain clear for an extended period after treatment. When prescribed by a dermatologist, oral isotretinoin can safely combine with hormonal and lifestyle therapies for better results.
At DermOnDemand, board-certified dermatologist Dr. Alicia Atkins explains that Accutane can be life-changing for patients with PCOS and acne who have not improved with other medications. Under expert care, the treatment is safe, effective, and tailored to each woman’s individual needs.
Key Takeaways
- Accutane (isotretinoin) effectively treats acne caused by hormonal imbalance in women with PCOS, reducing oil production, inflammation, and clogged pores when other treatments fail.
- While Accutane doesn’t correct hormone levels directly, combining it with therapies like oral contraceptives or spironolactone helps maintain long-term balance and prevent acne relapse.
- Dermatologists closely monitor blood and hormone levels during treatment to ensure safety, adjusting dosage and skincare plans based on each patient’s progress.
- Low-dose isotretinoin, combined with healthy lifestyle habits such as balanced nutrition, stress management, and gentle skincare, helps sustain clear, smooth skin after treatment.
- DermOnDemand offers personalized, online dermatology care under the guidance of Dr. Alicia Atkins, providing patients with professional isotretinoin guidance and follow-up support without the need for in-office visits.
How Accutane and PCOS Acne Are Connected
Why Women with PCOS Are More Prone to Acne
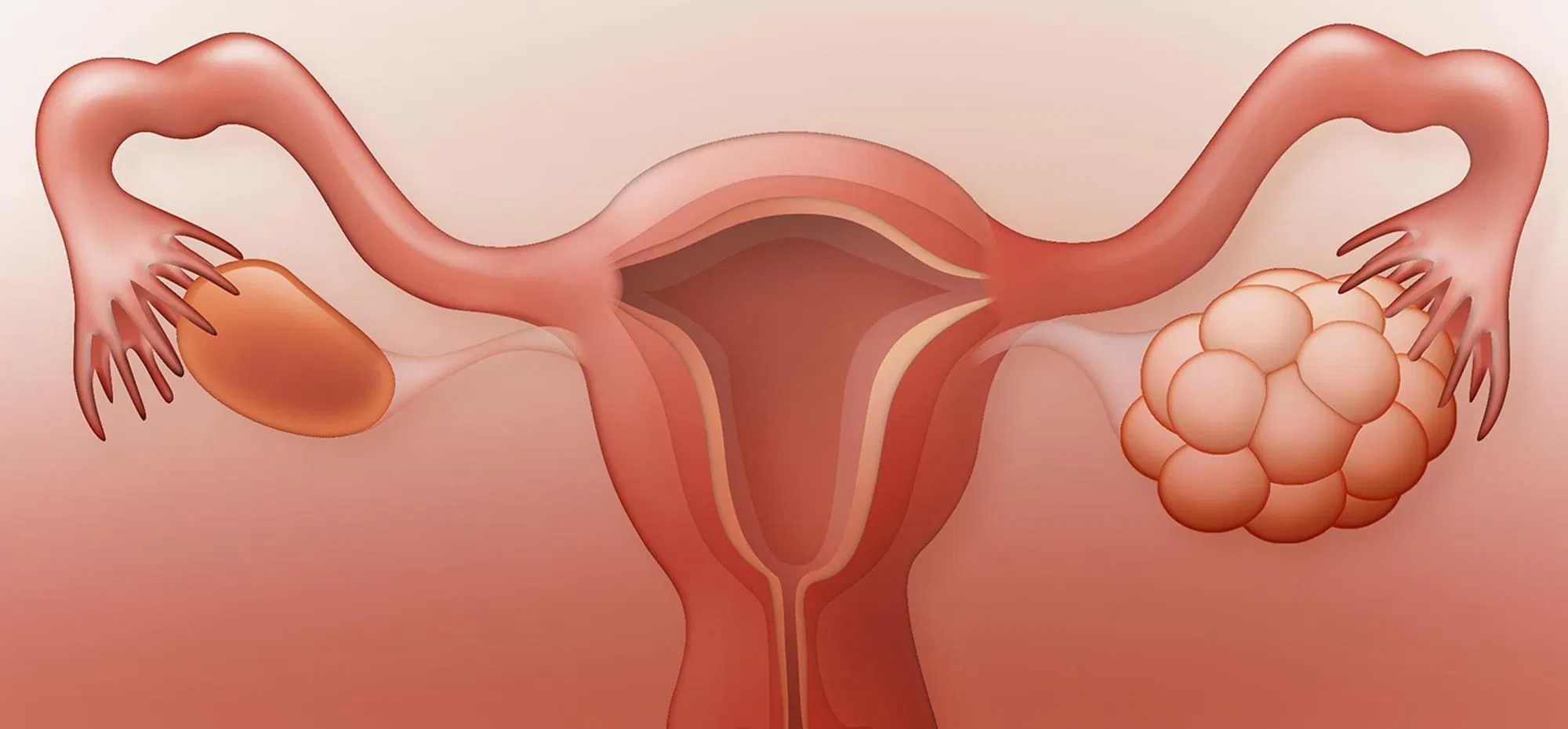
Women with polycystic ovary syndrome (PCOS) often produce higher amounts of androgens, which are male hormones like testosterone. These hormones cause the skin’s oil glands to become overactive, resulting in excessive oil production. When oil mixes with dead skin cells, it clogs pores and triggers acne vulgaris.
This hormonal imbalance also contributes to the development of small cysts in the ovaries and irregular menstrual cycles.
Hormone fluctuations throughout the month make acne worse around the chin and jawline. These are common areas for hormonal breakouts. Because the root cause is internal, topical creams or over-the-counter products rarely solve the issue.
PCOS-related acne requires a plan that treats both the skin and the hormones causing the imbalance.
Isotretinoin for PCOS Acne – How It Works
Isotretinoin, also known as Accutane, is a vitamin A derivative that targets the primary causes of acne. Unlike topical retinoids, the effects of isotretinoin and tretinoin differ in depth and potency, with oral isotretinoin working internally to regulate oil gland activity and reduce inflammation.
It shrinks the skin’s oil glands, reduces oil production, clears pores, and lowers inflammation. With less oil, the skin becomes smoother, pores appear smaller, and breakouts decrease.
For women with PCOS and acne, isotretinoin helps minimize how the skin reacts to high testosterone levels. It does not directly address hormonal imbalance, but it calms the skin’s response.
When paired with oral contraceptives or anti-androgen medication, oral isotretinoin delivers long-lasting improvements and clear, balanced skin.
Most patients begin to notice changes within 6–8 weeks, with full results typically appearing after several months. Even after stopping, many women remain clear for years because Accutane targets acne at its root.
Results and Safety of Accutane Treatment
Does Accutane Help with PCOS? Clinical Evidence
Yes. Research shows that isotretinoin treatment can significantly improve acne linked to polycystic ovary syndrome (PCOS). The medication works by reducing excess oil, shrinking the sebaceous glands, and calming inflammation, all key triggers of hormonal acne.
In one clinical trial, women with PCOS who used isotretinoin for six months experienced a reduction of up to 70% in acne lesions, fewer visible cysts, and a smoother skin texture.
When acne and polycystic symptoms are treated early, patients can prevent long-term issues such as scarring and uneven pigmentation. Dermatologists often pair Accutane with oral contraceptives or spironolactone to keep hormones stable and avoid new breakouts.
This combined plan offers more balanced skin and longer-lasting results, especially when guided by expert supervision.
What Research Says About Accutane and PCOS
Scientific research continues to explore how isotretinoin interacts with the hormonal changes seen in polycystic ovary syndrome (PCOS). Several clinical studies show that isotretinoin not only reduces oil and inflammation but may also slightly improve androgen sensitivity in the skin.
This means that while it doesn’t directly affect hormones, it helps the skin respond more normally to testosterone.
In one published study, women with PCOS who used isotretinoin for six months showed a marked reduction in sebum levels and acne severity. A few small studies have also observed improved insulin sensitivity and lipid balance, suggesting indirect metabolic benefits; however, more research is needed.
By translating this evidence into real-world care, Dr. Alicia Atkins and her team at DermOnDemand help patients understand what the data truly means: fewer breakouts, better skin texture, and a safer, more predictable treatment journey.
Does Accutane Affect Hormones in Women?
During isotretinoin therapy, dermatologists carefully monitor blood samples and hormone levels to ensure patient safety. Studies have shown that Accutane does not cause permanent changes to estrogen or testosterone levels. Its action is limited to the oil glands rather than hormone production.
Some women may experience mild changes in their menstrual cycle or dryness during treatment, but these effects are typically temporary. Dr. Alicia Atkins emphasizes that regular follow-ups and testing are crucial to ensure a safe and comfortable treatment.
At DermOnDemand, each plan is customized, and lab tests are reviewed at every stage.
Can Accutane Cause Ovarian Cysts or Change the Menstrual Cycle?
There is no scientific evidence showing that Accutane causes ovarian cysts or worsens PCOS. The medication only affects the skin’s oil glands. Some women may notice minor changes to their menstrual cycle, such as lighter bleeding, but these effects are temporary.
Patients may also experience mild side effects from isotretinoin, such as dryness, fatigue, or lip irritation, which typically resolve after treatment is completed.
At DermOnDemand, patients undergo a physical examination and gynecologic evaluation before starting isotretinoin. These tests confirm that the patient’s ovaries and hormones are stable.
Even women with existing small cysts can safely take Accutane when supervised by a dermatologist. Open communication during follow-ups ensures treatment remains safe and effective.
Medical Use and Recommended Dosage

Can You Take Accutane If You Have PCOS?
Yes. Women with polycystic ovary syndrome (PCOS) can safely take Accutane when other treatments don’t help. Before beginning, dermatologists review the patient’s medical history, order blood samples, and check hormone levels to confirm suitability.
Because isotretinoin can cause congenital disabilities, women must use reliable birth control, such as oral contraceptives, during treatment and for at least one month afterward.
Common side effects include dryness, mild fatigue, or mood changes, but they are temporary and manageable. Under medical care, Accutane is a trusted method for managing PCOS and acne effectively.
Low-Dose Accutane for PCOS – When It’s Recommended
A low-dose isotretinoin plan is ideal for women with sensitive skin or moderate acne. Lower doses reduce dryness, improve comfort, and minimize side effects. While results may appear slower, the long-term outcomes are just as strong as higher doses.
Dr. Alicia Atkins adjusts the dosage for each patient based on blood test results and progress. This enables safe and controlled improvement over time. Many women find low-dose therapy a perfect balance, gentle on the skin yet powerful against treated acne.
Medical Follow-Up During Treatment
Regular medical checkups are essential during isotretinoin therapy. Most dermatologists schedule visits every 4–6 weeks to review the skin’s progress, check blood samples, and monitor hormone levels. These appointments help detect early side effects such as dryness, sensitivity, or tiredness.
Patients who follow their appointments and skincare plan typically experience steady and predictable improvement. Close monitoring also ensures that oral isotretinoin stays safe and effective throughout treatment. At DermOnDemand, this careful follow-up helps maintain comfort and strong results.
How Dermatologists Monitor Safety During Accutane Therapy
Safety is central to every isotretinoin treatment. Dermatologists track several factors through regular testing and patient communication:
- Blood samples to monitor liver enzymes, cholesterol, and triglyceride levels.
- Hormone levels are checked to ensure the medication doesn’t interfere with estrogen or testosterone balance.
- Pregnancy prevention through the use of reliable contraception, since isotretinoin can cause congenital disabilities.
- Skin hydration checks to adjust moisturizers or supportive skincare as needed to address dryness.
At DermOnDemand, patients complete these steps from the comfort of their own homes through digital lab reviews and follow-up messages. This ongoing supervision provides peace of mind, ensuring every stage of treatment remains safe, transparent, and effective.
Alternative and Complementary Treatments
What Is the Best Acne Medication for PCOS?
Not every woman with PCOS-related acne needs Accutane. The best treatment depends on the severity of the acne and how hormones affect the skin. Several options can be effective when guided by a dermatologist:
- Oral contraceptives – help regulate the menstrual cycle and reduce androgen levels, which lowers oil production and prevents hormonal breakouts.
- Spironolactone – blocks the effect of excess testosterone on the skin, reducing oil buildup and inflammation.
- Topical treatments – products with retinoids or benzoyl peroxide help unclog pores and clear mild to moderate acne.
- Lifestyle changes, including a balanced diet, regular exercise, and stress management, support hormone stability and enhance skin health.
In most cases, dermatologists recommend a combined approach that treats both the hormonal cause and the visible acne. When these treatments are personalized and monitored, women with PCOS and acne can achieve lasting improvements and healthier, more balanced skin.
Accutane vs. Hormonal and Topical Therapies
Accutane targets the oil glands in the skin, reducing sebum production, inflammation, and clogged pores. Hormonal treatments, on the other hand, address the internal imbalance, such as high androgen and testosterone levels, that causes acne in women with PCOS.
Each therapy tackles a different part of the problem, and together they deliver stronger, longer-lasting results.
For example, oral isotretinoin clears active breakouts and prevents new ones from forming, while oral contraceptives regulate hormones and reduce excess oil. Topical treatments, such as retinoids or antibacterial creams, can further support daily skin care by keeping pores clean and calm.
At DermOnDemand, dermatologists frequently collaborate with endocrinologists to develop personalized plans that address both internal hormone balance and external skin health. This combined approach helps prevent relapse, smooths skin texture, and promotes lasting clarity.
Dermatologist Tips for Clear, Healthy Skin
Maintaining healthy skin after isotretinoin treatment is straightforward when you adopt consistent daily habits. These small steps help maintain your results and prevent new breakouts:
- Cleanse gently twice a day with a mild, non-foaming cleanser to remove oil and buildup without irritating the skin.
- Avoid heavy makeup and oily skincare products that can block pores and trigger breakouts.
- Apply sunscreen daily to protect against sun damage, redness, and the development of dark spots.
- Moisturize regularly with fragrance-free, non-comedogenic creams to restore hydration and reduce dryness.
- Never pick or squeeze pimples, as this can cause inflammation and lead to scarring.
- Schedule regular follow-ups with your dermatologist to adjust your skincare routine as your skin changes and evolves.
These habits, combined with professional guidance, keep your skin balanced, smooth, and healthy long after your treated acne has cleared.
Patient Experience and Relapse Prevention

How I Cured My PCOS Acne – Realistic Expectations
Most women begin to see visible improvements between the third and fifth month of isotretinoin treatment. The skin becomes less oily, pores shrink, and breakouts appear less frequently, healing more quickly.
Still, because acne and polycystic symptoms are linked to internal hormones, some women may need continued hormonal therapy to maintain clear skin in the long term.
With DermOnDemand, clear skin and confidence are just one consultation away. Learn more about our personalized acne treatment dermatologist services designed to deliver professional care and long-lasting results.
Dr. Alicia Atkins and her dermatology team closely monitor each patient’s progress, review lab results, and adjust doses or skincare plans when needed. This digital model makes consistent medical care convenient, ensuring that every patient receives ongoing support and achieves lasting, healthy skin.
PCOS Accutane Relapse – What to Do If Acne Returns
A few women may experience a PCOS Accutane relapse several months after finishing treatment. This usually occurs when hormone levels shift again or when stress, diet, or lifestyle changes disrupt the skin’s balance.
If acne returns, dermatologists may recommend a short maintenance cycle of oral isotretinoin or add hormonal support, such as spironolactone or oral contraceptives, to stabilize androgen levels.
To lower the chance of relapse:
- Follow a gentle skincare routine that keeps pores clear without irritation.
- Avoid touching or picking pimples, as this can worsen inflammation.
- Manage stress through relaxation or regular exercise.
- Maintaining a balanced diet and a healthy weight can help regulate hormone levels.
These practical steps, combined with professional follow-up, help maintain clear skin and reduce the risk of new flare-ups over time.
Post-Treatment Care and Skin Maintenance
After completing isotretinoin treatment, the skin becomes more sensitive and needs gentle care to stay healthy. A simple, consistent routine helps preserve your results and prevent new breakouts:
- Use mild retinoids a few times per week to keep pores clear and maintain smooth texture.
- Moisturize daily with lightweight, non-comedogenic creams to strengthen the skin barrier and prevent dryness.
- Avoid harsh scrubs or alcohol-based toners, which can irritate healing skin.
- Eat a nutrient-rich diet that includes fruits, vegetables, and omega-3 fatty acids to support skin repair.
- Exercise regularly to boost circulation and promote hormonal balance.
Maintaining stable testosterone levels and menstrual cycles, through medical guidance or lifestyle adjustments, plays a crucial role in preventing new acne flare-ups. With patience and daily consistency, your skin stays clear, balanced, and healthy long after treatment ends.
Frequently Asked Questions about Accutane and PCOS
Isotretinoin does not affect fertility, but it can cause severe congenital disabilities if pregnancy occurs during treatment. Women must use reliable contraception and avoid pregnancy for at least one month after stopping Accutane.
Yes, Accutane can safely be combined with oral contraceptives and other medications under a dermatologist’s care. Birth control helps control hormones, reducing flare-ups caused by PCOS and acne. Always inform your doctor before adding new treatments.
Accutane is usually continued until the skin remains clear for several weeks. If acne returns, dermatologists may suggest a second low-dose course or supportive therapy. Never restart oral isotretinoin without consulting a doctor.
At DermOnDemand, Dr. Alicia Atkins and her expert team of board-certified dermatologists provide safe, modern care for women with acne and polycystic ovary syndrome (PCOS) conditions. Through secure online consultations, patients can receive lab reviews, prescriptions, and follow-up plans within 24 hours.
The clinic’s mission is straightforward: to provide clear, science-based solutions for hormonal acne, without lengthy waits or clinic visits. With DermOnDemand, patients gain access to professional care tailored to their lifestyle, helping them achieve clear, confident skin through trusted medical treatments.