What is Melasma?
Melasma is a common disorder of hyperpigmentation characterized by gray-brown patches on the face, mainly the cheeks, chin, nasal bridge, and forehead. Women of color with darker skin tones, particularly from East Asia, Latin America, and Africa, are typically affected. Men and patients with lighter skin tones are less commonly affected.
What are the causes of melasma?
There are multiple causes of melasma. Ultraviolet (UV) exposure, genetic predisposition, pregnancy, and certain medications have been linked with melasma. Sunlight exposure is an important factor in melasma. UV exposure triggers the increase in production of melanin in melanocytes located on the face, neck, and arms. Some individuals may have a higher risk of getting melasma based on family history. Studies have shown that people with melasma are about 50% more likely to have a relative with melasma. In pregnancy, the increase in estrogen and progesterone hormones has been shown to cause melasma, also known as the “mask of pregnancy”. Certain medications, which include some antibiotics and topical retinoids, which increase the sensitivity of the skin to sunlight may cause melasma in some individuals.
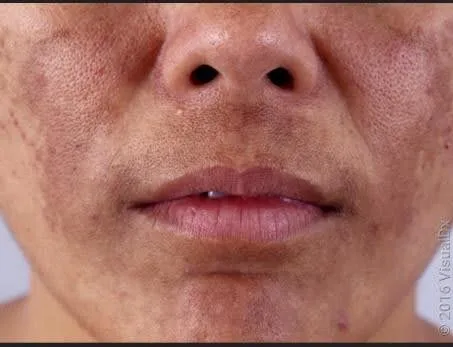
How does it look like?
Melasma causes skin discoloration by producing spots darker than the natural skin tone on both sides of the face, nose, cheeks, and jawline. Less commonly, melasma can appear on the neck and sun-exposed arms. Melasma does not cause pain or itching.
How is melasma diagnosed?
A diagnosis is made through clinical examination by a physician. In some cases, a dermatologist may use a Wood’s lamp, a handheld light device, to appropriately localize areas of dyspigmentation.
What are treatment options?
The goals of treatment are to prevent the production of melanin the skin makes and restore it to the natural skin tone. Photoprotection is the most important therapy to prevent worsening of melasma. Tinted sunscreens (with SPF 30 or higher) containing iron and titanium oxides are recognized as efficient methods of protection from UV and visible light. Some sunscreen formulations also possess benefits that allow for concealment of dark spots which can be incorporated into daily skincare regimens.
The treatment for melasma is a triple combination cream consisting of three medications: hydroquinone, retinoids, and corticosteroids. Other topical creams like cysteamine and tranexamic acid have been used to decrease skin discoloration. Tranexamic acid is also available as a pill and has been shown to effectively reduce dark spots in melasma. Sometimes, a board-certified dermatologist may combine procedures like lasers, chemical peels, and microneedling in addition to topical creams to maximize results. It may take up to 12 months to see the results from treatment, so camouflage makeup is encouraged until melasma fades.